
BLOG
Inspiration for your movement and parenting journey.

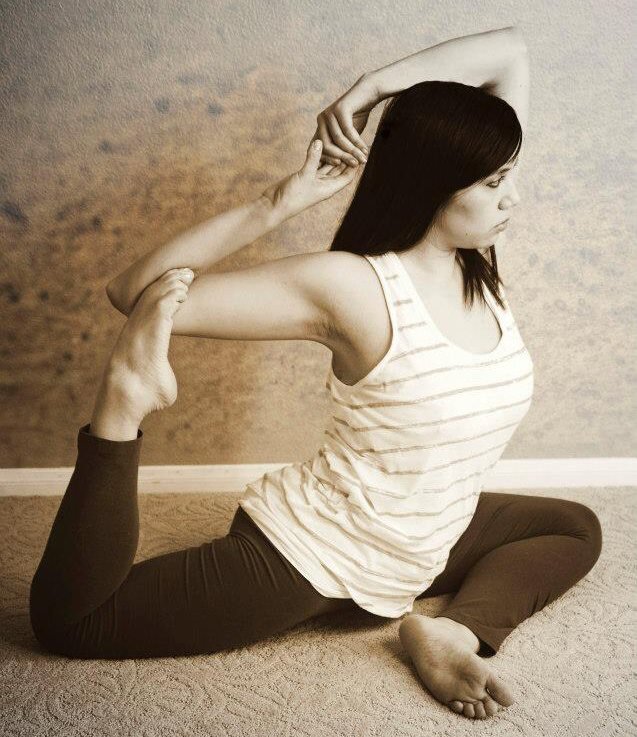
Yoga for Pelvic Health: Managing Stress Incontinence
Dealing with stress incontinence can be challenging, affecting both men and women. In this blog post, we'll explore what stress incontinence is, its causes and contributing factors, and most importantly, how yoga and movement can be a valuable tool in managing pelvic health.
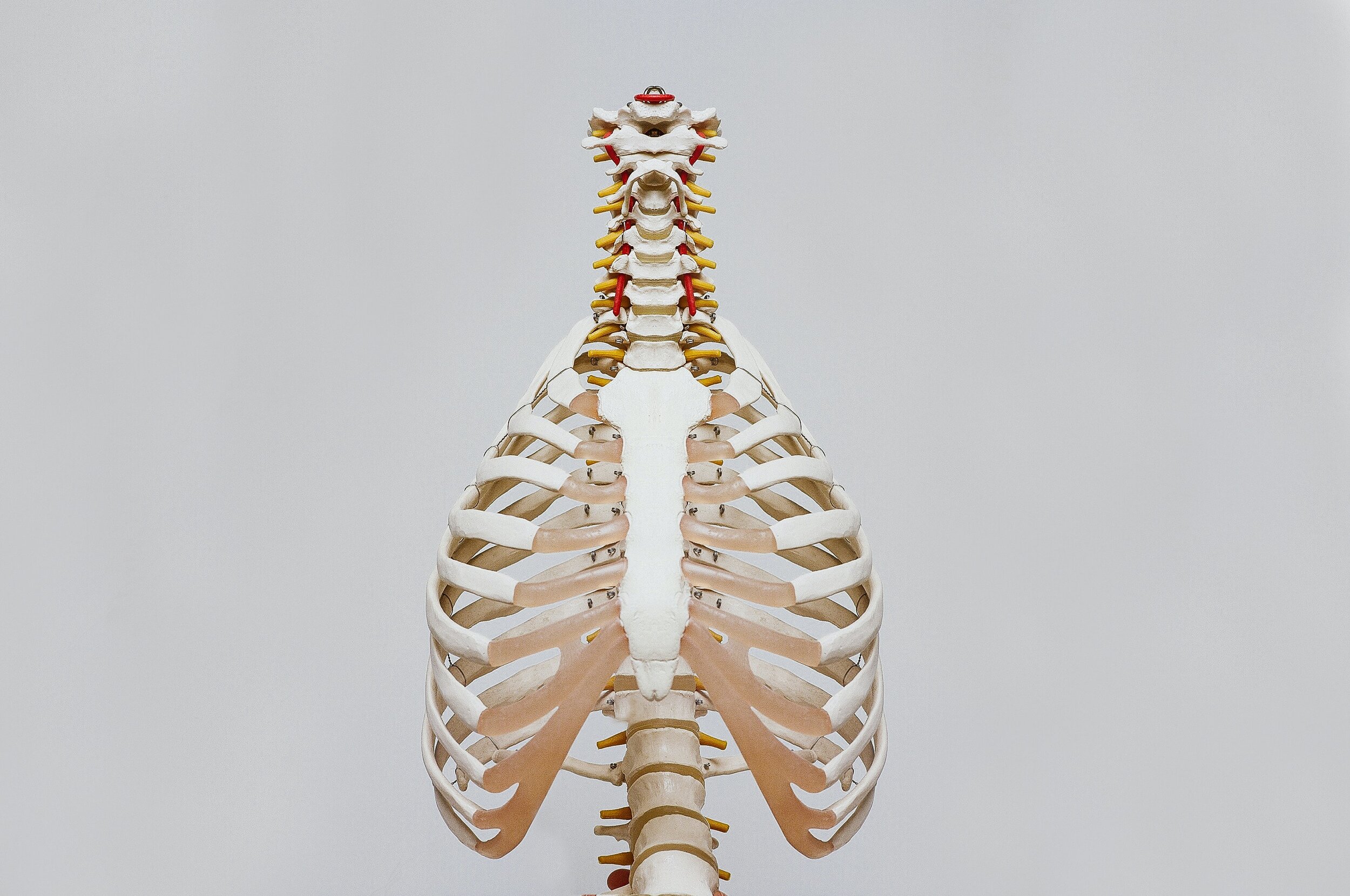
Rib Cage Breathing
Rib cage breathing is the main breath taught at Prenatal Yoga Las Vegas because it is optimal for pregnancy and beyond. Chest breathing tends to be short and shallow and belly breathing heavy focus on breathing downward can compromise a weak pelvic floor. Rib cage breathing focuses on expansion throughout the sides, front and back of the lungs.

What is Pelvic Floor Physical Therapy and Who Needs it?
Pelvic health, or pelvic floor, physical therapy is a niche of physical therapy for both women and men that focuses on the pelvis and pelvic floor, hips, low back, and abdominals. The pelvic floor is the layer of muscles that covers the bottom of the pelvic cavity (think of the area that touches the seat when you ride a bike) that supports the organs within the pelvis, aids in functions related to urinating and defecating, and assists in sexual function.
The Story of My Pelvis
The story of our pelvis is a combination of what we learn from our families, friends and media, the actions of others, and our physical health. Messages about our menstural cycle and sexuality are especially important. Sexual assult is so common in American society, I can't help but wonder the cumulative effects. Naturally if part of the body has been injured or hurt, there is a natural guarding. After years of guarding, the muscles shorten and become tense. Our pelvic floor muscles work in tandem with other muscles groups. Tightness in one area can affect the entire system.

Why is pelvic health important?
When I start to talk about pelvic health, most people think that pelvic health is exclusively related to leaking and/or women problems. If you're not someone who is currently leaking, you may write yourself off from pelvic health altogether. However, pelvic health is so much more than that!

Yoga for Pelvic Girdle Pain
Pelvic girdle pain (PGP) is one of the most common complaints I hear from my prenatal students. PGP varies in severity and areas of pain. PGP maybe a persistent on-going pain or triggered by certain movements, or a combination of both.

The Truth About Diastasis Recti And What You Can Do About It
Diastasis recti (dahy-as-tuh-sis rek-tahy) is the displacement of the abdominal wall muscles. Diastasis recti is the partial or complete displacement of the rectus abdominis, or “six-pack” muscles, which meet at the midline of your stomach. Diastasis recti is very common during and following pregnancy. This is because the uterus stretches the muscles in the abdomen to accommodate your growing baby.
